Update on CAR T-Cell Therapies for the Treatment of Cancer
Let’s start with the source of the cells being modified. In general, there are two categories of CAR immune cells: Autologous and Allogeneic. Autologous CAR therapies are derived from the patient’s own cells while allogeneic CAR therapies are typically taken from healthy donors and given to a different recipient. Both classes have pros and cons and are potentially powerful tools in the fight against cancers.
Autologous vs. Allogeneic
Since autologous CAR therapies are derived from the patient’s own cells there is inherently less risk that the patient will reject the cells. In addition, autologous CAR therapies have a lower risk of the cells rejecting the patient (Graft-versus-host disease [GVHD]). Since the patient is receiving their own cells back (but modified) there is an assumption that these modified cells are safer for the patient since the cells originated from them in the first place.
However, there is one potential drawback. If the extracted cells are not coming from a healthy individual, by definition, and are fundamentally flawed due to specific underlying health conditions, the cells may not be as efficacious as other cells. Typically the modifications to the cells are intended to overcome this issue, but it has to be considered that the source of the cells may not be the optimal immune cells to choose.
In the case of allogeneic cells, since the cells are taken from someone other than the receiving patient, there is some risk that the patient will reject those cells or the cells will reject the patient. A comparative situation that most people are familiar with is the challenges that come along with solid organ transplants.
Similar to the tools developed to help patients receive transplants, these can be utilized to overcome the “mismatch” associated with receiving someone else’s cells. And although the primary modification to the cell is to add the CAR, additional modifications can be made to assist in this “mismatch.” The upside for allogeneic cells is that the cells come from (typically) younger, healthier donors. These cells may be more optimal immune cells for fighting the cancer. The modifications made by adding in the CAR and other edits result in a super-charged cell that fights the cancer.
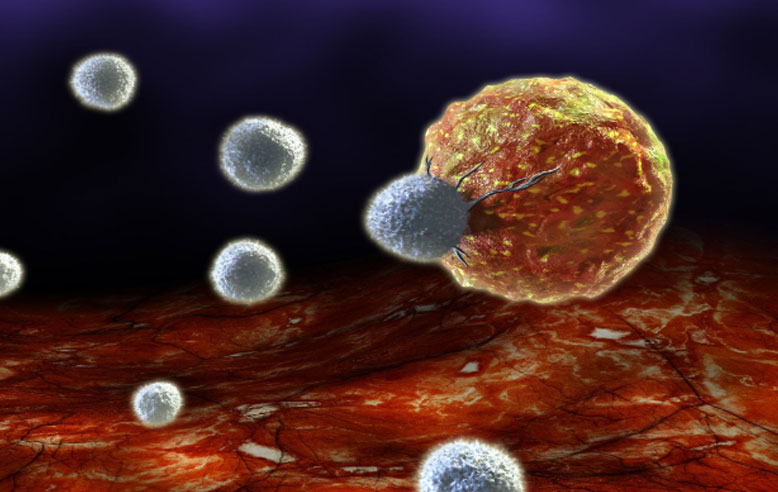
In either case, the intent is to provide the patient with an immune cell that can increase in number (proliferate) following delivery, go to the tumor, and attack it with the hope of reducing tumor burden. Or, in the best possible case, completely eliminating the cancer altogether.
CARs Aren’t Just for T Cells Anymore
If you are familiar with CARs, you may be wondering why we haven’t referenced a CAR T-cell so far. Although many think of T cells when discussing gene-edited cell therapies, the technology is branching out into a number of cell types. B Cells, NK cells, and Macrophages are all now being edited for a similar purpose as CAR T cells.
It’s probably important to note that these cells aren’t just being edited to incorporate the CAR alone. Instead, a wide array of changes can be incorporated to provide a more appropriately functioning immune cell for combating cancer. Edits to reduce immunogenicity, prolong the lifespan of the immune cell and better persistence of the edited cell can all be performed to create a more potent anti-cancer immune cell to deliver to the patient.
Current CAR T-Cell Therapy Approvals
The number of FDA-approved CAR T cell therapies is growing and we can expect this list to rapidly increase in the coming years. Here are the 4 FDA-approved therapies available to patients:
- Kymriah™ (tisagenlecleucel): Kymriah has been shown to be effective in treating B cell precursor acute lymphoblastic leukemia (ALL) in children and young adults up to the age of 25 years of age when combined with chemotherapy. Acute lymphoblastic leukemia is the most common cancer and the leading cause of death-related cancer in children.
- Yescarta™ (axicabtagene ciloleucel): Yescarta, which was initially approved for treatment in adults with diffuse large B-cell lymphoma and granted accelerated approval in Feb 2021 as a treatment option for follicular lymphomas, has also been indicated to be effective against Mantle Cell Lymphoma (MCL).
- Tecartus™ (brexucabtagene autoleucel): Formerly KTE-X19, became available in July 2020. Tecartus has become one of the newest treatments offered by physicians caring for people living with difficult cancers like advanced Mantle Cell Lymphoma (MCL).
- Breyanzi (lisocabtagene maraleucel): The Food and Drug Administration (FDA) approved Breyanzi for the treatment of adult patients with relapsed or refractory large B-cell lymphomas on February 5, 2021.
All 4 FDA-approved therapies are autologous CAR T-cells targeting CD19, an antigen found on the surface of B-cells.
What’s Next for CAR-edited cells?
The field is rapidly growing with new cell types, newly derived CARs targeting new proteins, with multiple edits being performed to create the next generation of CAR-edited cells. The expansive growth in this field has resulted in parallel growth in the bioanalytical tools needed for regulated support. Platforms like PCR and flow cytometry are now key tools for measuring the pharmacokinetics of a living drug. We should expect to see a greater emphasis on these platforms and the development of regulatory standards to support their use.
The potential impact for these therapies is without limit. The ability to apply the learnings from the oncology space into autoimmune and inflammatory diseases will be key steps to the continued growth of the gene-edited, cell therapy space.
Partner With BioAgilytix
BioAgilytix is privileged to contribute to the exciting and promising new field of immunotherapy by supporting innovative CAR T therapy programs. Working in collaboration with sponsors, we utilize our strengths in cell-based assays to assist with the characterization of these cells.
BioAgilytix provides biomarker, immunogenicity, cell-based assay, and other laboratory services for pharma and biotech companies around the world. We are a leader in immunogenicity testing, an important step in drug development, evaluating anti-drug antibodies prior to treatment, and analyzing drug efficacy in a patient over time. Contact BioAgilytix today with any questions or requests, or for information on our expertise in tumor/immune biomarkers or CAR T-cell therapy programs.
https://pubmed.ncbi.nlm.nih.gov/33499101/
https://docs.google.com/document/d/1ufh9crWcTw4gIuHxPYEz9UU6KyoAbUjpiSZzX6xBArw/edit#